A case report of Klebsiella aerogenes-caused lumbar spine infection ... - BMC Infectious Diseases
A 69-year-old woman was hospitalized on July 30, 2020, with recurrent fever without any cause for two weeks and continuous lower back pain for three days. Three months prior, she presented with chest discomfort and fatigue without an obvious cause, occasional chest pain after activity, and frequent urination at night. She did not have paroxysmal nocturnal dyspnea, fever, cough, expectoration, urinary pain, nausea, vomiting, abdominal pain, abdominal distension, or diarrhea. Physical examination revealed high inflammatory indices, including a white blood cell (WBC) count of 21.7 × 109 cells/L, a C-reactive protein (CRP) level of 12.46 mg/L, and procalcitonin (PCT) level of 0.19 ng/mL. She was treated for infection and anemia, as laboratory tests revealed an erythrocyte count of 1.00 × 1012/L, a hematocrit of 14.0%, a hemoglobin concentration of 43 g/L, a mean corpuscular volume (MCV) of 140.0 fL, a mean corpuscular hemoglobin (MCH) level at 43.0 Pg, and a MCH concentration of 307 g/L (Table 1). The symptoms did not improve, and the patient remained at our hospital for treatment.
The chief complaint at admission: In 2006, the patient underwent radical mastectomy and chemotherapy after surgery, with a 7-year history of hypertension and continuous lower back pain for three days. Through physical examination, it was found that the patient had back tenderness and paravertebral percussion pain, leading to the diagnosis of thoracic degenerative changes, particularly compression changes at the fifth and the twelfth thoracic as well as the third lumbar vertebra. Body temperature fluctuated between 38.6 and 38.8 °C, and the patient was treated with ceftriaxone and ceftazidime. On August 18, she was hospitalized again due to recurrent fever for 2 weeks and severe diarrhea for 1 day. Chest computed tomography (CT) revealed the absence of soft tissue shadows in the right breast and right armpit, increased texture in both lungs, a cord-like shadow in both lungs, a small amount of left pleural effusion, and bilateral pleural thickening (Fig. 1A).
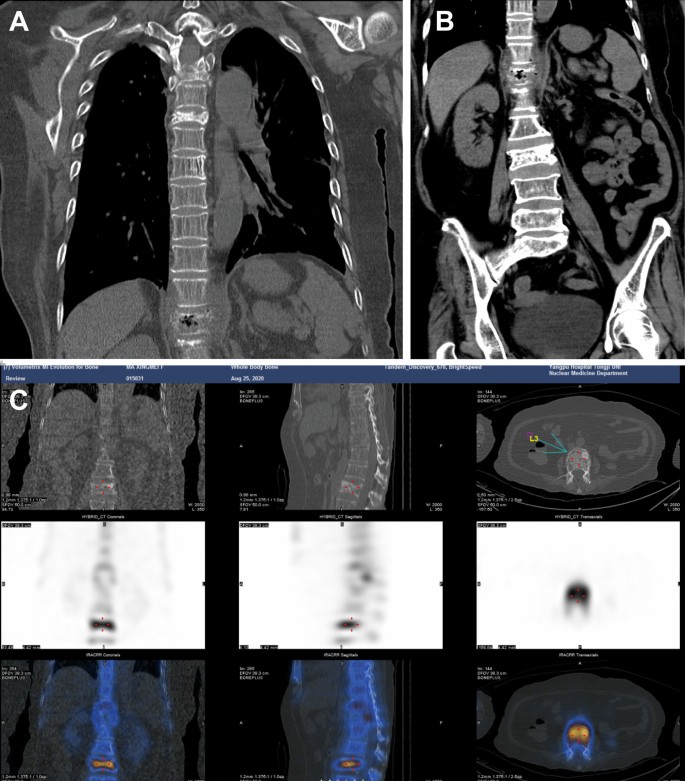
Thoracolumbar imaging findings. A Chest CT on August 18, 2020. B Abdominal CT on August 18, 2020. C Radionuclide scan on August 25, 2020
Abdominal CT showed a slightly enlarged spleen, local pneumatosis expansion in the proximal colon ascendens, and no other visible abnormalities (Fig. 1B). Blood cultures were positive for K. aerogenes within 15 h (Table 2), and the result of urine cultures was negative, while stool cultures were positive for Candida albicans and negative for Enterobacter sp. and Vibrio casei. Based on drug sensitivity testing and the patient's condition, meropenem and diflucan (fluconazole resistance) were administered against infection. Detailed information on the drug sensitivity testing was provided in the Additional file 1: Online Technical Appendix. After 4 days, body temperature was normal, and the patient was treated with sulperazon.
On August 25, the patient, who had a history of breast cancer, experienced chest discomfort. A bone scan with the whole-body bone scintigraphy was performed, confirming the absence of bone metastases, while also revealing cuneiform changes at the third, fifth, twelfth thoracic vertebrae, and the third lumbar vertebra, indicative of degenerative changes in the thoracolumbar spine (Fig. 1C). During follow-up from anemia treatment, the patient had a normal hemoglobin level and was administered oral prednisone at a dose of 10 mg bid. The patient's D-dimer levels remained high, and an improved pulmonary artery CT angiography (CTA) suggested that the small branch was embolized in the lower lobe of both lungs. The patient was treated with low-weight molecular heparin and switched to oral anticoagulants (rivaroxaban) when under stable condition.
On August 27, the patient returned to a normal body temperature, and antibiotics were discontinued. On August 31, the patient had increased PCT level, so she was once again treated with sulperazon against infection until she was discharged on September 12. There was no significant change in the blood routine and PCT indices during this period. She experienced a fever again without an obvious cause one day after discharge. Upon admission, the highest body temperature was 39.5 °C, accompanied by aversion to cold, chills, and fatigue. Physical examination revealed a CRP level of 88.89 mg/L, a WBC count of 14.4 × 109 cells/L, a body temperature of 40.4 °C, and shock. K. aerogenes infection was detected through blood cultures within 12 h, and the patient was subsequently treated with meropenem against infection.
A CT scan of the thoracoabdominal region showed significant changes in the twelfth thoracic vertebra. Abdominal CT revealed vertebral compression change of the third lumbar vertebrae. MRI of the lumbar spine showed bone destruction from the eleventh thoracic vertebrae to the first lumbar vertebrae, protrusion of the intervertebral disc at the fifth lumbar vertebra to the first sacral vertebra, and degenerative changes in the lumbar spine (Fig. 2A ). Therefore, we considered that the patient had a vertebral infection. The patient experienced recurrent vague back pain, which she tolerated over half a year. Considering bone destruction, the expert consultation from another hospital led to the administration of cefepime combined with levofloxacin for the treatment of infection. One day later, the patient once again had a fever, and the axillary temperature was 38.5 °C, with a CRP level of 47.9 mg/L and a WBC count of 14.6 × 109 cells/L. The antibiotic was changed to meropenem combined with moxifloxacin, and the following two times of blood cultures were negative.
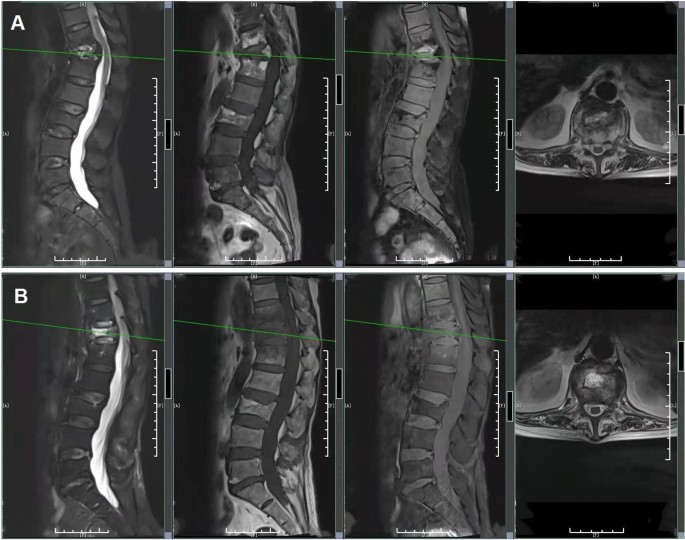
Results of the MRI in lumbar and thoracic vertebrae. A MRI of the lumbar and thoracic vertebrae on September 17, 2020. B MRI of the lumbar and thoracic vertebrae on October 10, 2020
On October 10, MRI of the lumbar spine revealed bone destruction from the eleventh thoracic vertebra to the first lumbar vertebrae. The thoracic MRI indicated mild deviation with signal changes of the eleventh thoracic vertebrae and the first lumbar vertebrae as well as vertebral compression with signal abnormalities of the twelfth thoracic vertebrae (Fig. 2B). From October 16 to 29, blood cultures were negative twice in a row, but K. aerogenes was detected via metagenomic next-generation sequencing (mNGS) on the 21st (Table 3). The specific methods of mNGS were described in the Additional file 1: Online Technical Appendix. Cefepime and moxifloxacin were administered continuously. The patient's body temperature and inflammatory indexes tended to be normal during the treatment. After discharge, the patient continued oral administration of levofloxacin as well as doxycycline for infection treatment and was instructed to rest in bed to prevent falls, avoid stress on the waist, and appropriately move the lower limbs to avoid thrombosis. During the follow-up period, routine blood tests, inflammatory indexes, and body temperature were normal.
Comments
Post a Comment